The Basics. What PMS Is And What It Isn't
This article explores what PMS is, what else your symptoms could be, if lab testing is really necessary and some tricks for finding some relief.
WOMEN'S HEALTH
Dr. Ali McMillan ND
8/24/202512 min read
You have no doubt heard a lot about Premenstrual Syndrome (PMS) at this point in your life. It’s a common syndrome, commonly referred to in the media and often inferred upon a woman whether they have it or not. It is such a well-known condition that people feel comfortable applying it to women universally and diagnosing themselves or others at whim.
But PMS is a bit more nuanced than common knowledge would have you believe. There are many widely circulated myths about PMS, and research continues to teach us more and more about this somewhat misunderstood condition.
First, PMS is a syndrome with a very large list of potential symptoms. To be diagnosed with PMS, a menstruating person needs to have both mood-related symptoms and physical symptoms during the luteal phase that negatively impact their life. Let's unpack this.
Requirements for a PMS diagnosis
1. Symptoms
You must have mood and physical symptoms, usually at least one of each from the list below. Everyone thinks about cramps and mood swings, but there are many others, and cramps seem to be missing entirely. This list is from a validated symptom tracker.
Physical Symptoms:
Joint or muscle pain
Headaches
Breast swelling
Feeling bloated
Weight gain
Have trouble getting to sleep or staying asleep
Sleep more, take more naps, find it difficult to get up when intended
Feel lethargic, fatigued or lacking energy
Specific food cravings
Increased appetite
Mood Symptoms
Feel depressed, sad, down or blue
Feel hopeless, out of control or overwhelmed
Feel worthless of guilty
Feel anxious, tense, keyed up, on edge
Have mood swings (suddenly feel sad or tearful)
Feel more sensitive to rejection
Feelings are more easily hurt
Feel angry or irritable
Have conflicts or problems with people
Have less interest in work, school, friends or hobbies
Have difficulty concentrating
2. Timing
The symptoms must occur during the luteal phase. The luteal phase is the stretch of time between ovulation, which occurs around day 14 (quite variable) and extends until the first day of menstrual flow. For many, this is a span of about 2 weeks. You can have symptoms just before menses, but some people have symptoms for the whole two weeks. It is quite a range.
If these symptoms occur before ovulation, in the follicular phase, this could be a different condition that is worsened by normal hormonal change. We use trackers to help sort this out.
3. Impact
The symptoms must negatively impact your life.
This requirement is interesting. Even minor pain can significantly impact some people's lives. The tracker defines this impact as follows…
“At work, school, home, or in daily routine, at least one of the problems noted above caused reduced productivity or inefficiency.”
“At least one of the problems above interfered with hobbies or social activities.”
“At least one of the problems above interfered with relationships with others”
I must note, the ability to power through the symptoms, despite being uncomfortable, emotional, etc., does not disqualify someone as needing treatment or being diagnosed.
Over the next few weeks, I will be publishing more information I want people to know about PMS. If you have PMS or premenstrual symptoms and need support, I am happy to see you in the office. Just click one of the Book Now buttons to book an appointment.
References
Vaghela N, Mishra D, Sheth M, Dani VB. To compare the effects of aerobic exercise and yoga on Premenstrual syndrome. J Educ Health Promot. 2019 Oct 24;8:199. doi: 10.4103/jehp.jehp_50_19. PMID: 31867375; PMCID: PMC6852652.
Mohebbi Dehnavi Z, Jafarnejad F, Sadeghi Goghary S. The effect of 8 weeks aerobic exercise on severity of physical symptoms of premenstrual syndrome: a clinical trial study. BMC Womens Health. 2018 May 31;18(1):80. doi: 10.1186/s12905-018-0565-5. PMID: 29855308; PMCID: PMC5984430.
Houghton SC, Manson JE, Whitcomb BW, Hankinson SE, Troy LM, Bigelow C, Bertone-Johnson ER. Carbohydrate and fiber intake and the risk of premenstrual syndrome. Eur J Clin Nutr. 2018 Jun;72(6):861-870. doi: 10.1038/s41430-017-0076-8. Epub 2018 Jan 29. PMID: 29379144; PMCID: PMC5990431.
Sayegh R, Schiff I, Wurtman J, Spiers P, McDermott J, Wurtman R. The effect of a carbohydrate-rich beverage on mood, appetite, and cognitive function in women with premenstrual syndrome. Obstet Gynecol. 1995 Oct;86(4 Pt 1):520-8. doi: 10.1016/0029-7844(95)00246-n. PMID: 7675373.
Hashim MS, Obaideen AA, Jahrami HA, Radwan H, Hamad HJ, Owais AA, Alardah LG, Qiblawi S, Al-Yateem N, Faris MAE. Premenstrual Syndrome Is Associated with Dietary and Lifestyle Behaviors among University Students: A Cross-Sectional Study from Sharjah, UAE. Nutrients. 2019 Aug 17;11(8):1939. doi: 10.3390/nu11081939. PMID: 31426498; PMCID: PMC6723319.
Casper, R. Feb 4th 2021. Patient education: Premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD) (Beyond the Basics). UpToDate.
Steiner M. Premenstrual syndrome and premenstrual dysphoric disorder: guidelines for management. J Psychiatry Neurosci. 2000 Nov;25(5):459-68. PMID: 11109297; PMCID: PMC1408015.
Bhuvaneswari K, Rabindran P, Bharadwaj B. Prevalence of premenstrual syndrome and its impact on quality of life among selected college students in Puducherry. Natl Med J India. 2019 Jan-Feb;32(1):17-19. doi: 10.4103/0970-258X.272109. PMID: 31823933.
Sayegh, R., Schiff, I., Wurtman, J., Spiers, P., McDermott, J., & Wurtman, R. (1995). The effect of a carbohydrate-rich beverage on mood, appetite, and cognitive function in women with premenstrual syndrome. Obstetrics and Gynecology, 86(4 Pt 1), 520–528.
Wurtman, J. J. (1990). Carbohydrate craving. Relationship between carbohydrate intake and disorders of mood. Drugs, 39 Suppl 3, 49–52.
Esmaeilpour, M., Ghasemian, S., & Alizadeh, M. (2019). Diets enriched with whole grains reduce premenstrual syndrome scores in nurses: An open-label parallel randomised controlled trial. The British Journal of Nutrition, 121(9), 992–1001. https://doi.org/10.1017/S0007114519000333
Premenstrual symptomatology and alcohol consumption in college women. Bridget L Perry, Donna Miles, Karen Burruss, and Dace S Svikis. Journal of Studies on Alcohol200465:4, 464-468
Fernández, M. del M., Saulyte, J., Inskip, H. M., & Takkouche, B. (2018). Premenstrual syndrome and alcohol consumption: A systematic review and meta-analysis. BMJ Open, 8(3). https://doi.org/10.1136/bmjopen-2017-019490
Caan B, Duncan D, Hiatt R, et al. Association between alcoholic and caffeinated beverages and premenstrual syndrome. The Journal of Reproductive Medicine. 1993 Aug;38(8):630-636. PMID: 8410870.
Bäckström T, Bixo M, Johansson M, Nyberg S, Ossewaarde L, Ragagnin G, Savic I, Strömberg J, Timby E, van Broekhoven F, van Wingen G. Allopregnanolone and mood disorders. Prog Neurobiol. 2014 Feb;113:88-94. doi: 10.1016/j.pneurobio.2013.07.005. Epub 2013 Aug 23. PMID: 23978486.
Nyberg, S., Andersson, A., Zingmark, E., Wahlström, G., Bäckström, T., & Sundström-Poromaa, I. (2005). The effect of a low dose of alcohol on allopregnanolone serum concentrations across the menstrual cycle in women with severe premenstrual syndrome and controls. Psychoneuroendocrinology, 30(9), 892–901. https://doi.org/10.1016/j.psyneuen.2005.04.016
If It's Not PMS, What Is It?
Most people assume they have PMS if they have specific symptoms or cyclical symptoms. But could it be something else?
Conditions That Mimic PMS
There are a number of conditions that look a lot like PMS but actually aren't. Treating PMS when a patient has a completely different condition wont help at all so determining what is really going on is important.
Common PMS mimicking conditions are...
Anxiety
Depression
Perimenopause (more of a normal phase of life than a condition)
Irritable bowel syndrome
Thyroid disease
Conditions That Can Get Worse in the Luteal Phase
Some conditions have a cyclical nature, and symptoms get worse during the luteal phase (between ovulation and menstruation) as these conditions are exacerbated by fluctuating hormones.
Common conditions exacerbated during the luteal phase include...
Anxiety
Depression
Migraines
Epilepsy
Allergies and Asthma
All these conditions, the mimics and the exacerbators, can also co-exist with PMS, adding another layer of potential complexity.
How Can You Tell What Is PMS, A Mimic, An Exacerbator or A Combination?
Human health is complicated, but symptom trackers can really help untangle this particular set of conditions. The tracker I suggest to my patients has been validated in studies and is on paper to keep health information private. Tracking should be done for about 3 months to get a clear picture, but this should not delay treatment. You can track and treat at the same time.
A few of these conditions, like hypothyroidism, are also easily ruled out with basic blood tests. Often, there are other conditions considered for a patient based on their unique presentation that may also need to be ruled out (like PCOS, Endometriosis, fibroids, etc.).
Blood Tests and PMS. Is There A Point?
No blood test can confirm or deny if someone is suffering from PMS. It would be nice if there were, but such a test simply doesn't exist. For a long time, people would test sex hormone levels (like estrogen and progesterone) are various points in the menstrual cycle for clues, but sex hormone levels are largely the same in people who have PMS and people who don't. There are other reasons to test these hormones, but they don't diagnose PMS.

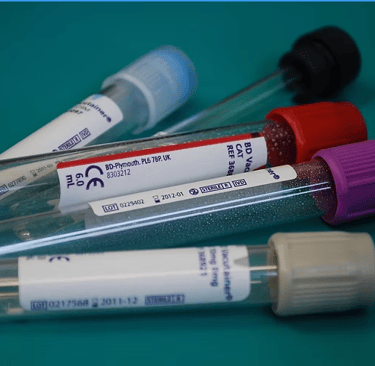
So if you can't diagnose PMS with a blood test, why run one?
Because of PMS mimicking conditions. I talked a bit about some examples of conditions that act like PMS above, and some conditions that are worsened by PMS. Some of these conditions can be ruled out with simple, inexpensive blood tests. Not all of these tests apply to all PMS patients.
Hypothyroidism can usually be ruled out with a TSH test
Anemia (common in people who menstruate) can be ruled out with a CBC and Ferritin
Prolactin can be tested to rule out a prolactinoma, which is a rare condition.
Vitamin D can be run to find a deficiency, which can make PMS symptoms a bit worse. Vitamin D deficiency is common in Canada.
FSH can look for premature ovarian failure and menopause, which is relevant in some cases.
17-OHP can help detect congenital adrenal hyperplasia. Is condition is rare.
Testosterone and blood glucose measures are sometimes tested to look for PCOS.
Sometimes estrogen and progesterone are useful to find information about the menstrual cycles, fertility, pregnancy and development through puberty if issues arise. Progesterone is useful to confirm that ovulation is occurring. Some people are reassured by testing these hormone levels.
I have never needed to order all of these tests for one patient. Typically, there are a few that, based on symptoms, will seem the most relevant for a patient. The first 4 listed are commonly ordered. There are others that come up depending on what patients are experiencing that are not listed here.
Self-Care Tips to Reduce PMS Symptoms
Premenstrual syndrome (PMS) is a condition that affects many women during their menstrual cycle. It can cause a variety of physical and emotional symptoms, including bloating, fatigue, irritability, and mood swings. While these options will not cure PMS, there are a number of self-care strategies that can help to alleviate symptoms and improve overall well-being.
1. Can Exercise Improve PMS?
I know this seems counterintuitive because most people don't feel like exercising when they have PMS symptoms, but hear me out. The exercise doesn't have to occur during PMS to reduce symptoms necessarily. People who exercise 3 times a week can reduce the pain they experience during the premenstrual phase of their periods. In one study, yoga worked a little better than aerobic exercise, but both worked. A drop in pain was observed after only one month of exercising 3 times per week for 40 minutes each time.
A more comprehensive study found that after 8 weeks of exercising 3 times per week for only 20 minutes, there was a reduction in nausea, constipation, diarrhea, swelling, bloating, vomiting and hot flashes.
Regular exercise can also help to reduce stress, improve mood, and increase energy levels. Aim for moderate exercise each day if you can, such as walking, jogging, or cycling.
2. Eat a Healthy Diet to Reduce Symptoms
Eating a healthy diet is important for managing PMS. Avoid processed foods and foods high in sugar and salt. High salt foods can contribute to water retention. Instead, focus on eating whole, nutrient-dense foods like fruits, vegetables, whole grains, and lean protein sources.
A diet that is high in calories/fat/sugar/salt has been identified as a strong risk factor for physical symptoms of PMS. High fruit consumption, on the other hand, was found to decrease behavioural symptoms. Fruit continues to be amazing.
3. Avoid Smoking
Smoking tobacco is strongly correlated with an increase in PMS symptoms. This makes sense. Smoking is very inflammatory, and pain is usually worsened by inflammatory issues. Smoking cessation can be a challenge, so seek out help if you need it.
4. Consider Heat Therapy
Applying heat to the lower abdomen can help to relieve cramps and bloating associated with PMS. Try using a heating pad or taking a warm bath to ease discomfort.
5. Should I Take Supplements?
There are some great options for PMS-relieving supplements. There are 2 that seem to have a lot more evidence than the others. But keep in mind, many herbs and supplements have been proven ineffective as well. Taking supplements should be done under the care of a qualified health care practitioner who will ensure that the supplements you take are likely to work, safe for you specifically and will not contradict any medication you happen to be on. Supplements also have the potential to cause side effects.
I check all herb and supplement prescriptions for interactions with the medication my patients are already taking and inform them of potential side effects. Side effects are rare, but it is important to know about them.
6. Connect with Others, Especially Women
Connecting with friends and family can help boost mood and alleviate stress associated with PMS. Make time to spend with loved ones, or consider joining a supportive group to connect with others who are experiencing similar symptoms. If your PMS symptoms are getting in the way of maintaining relationships, then you should seek some help from an ND, MD, counsellor or other qualified professional.
Self-care is an important part of managing PMS. By making healthy lifestyle choices, practicing stress management techniques, and connecting with others, you can help to alleviate symptoms and improve overall well-being. If your PMS symptoms are severe or interfering with your daily life, be sure to talk to your healthcare provider for additional support and treatment options.


3 Common Mistakes Patients With PMS Make
There is a lot of contradictory information on the internet and a lot of general assumptions that become adopted as "common knowledge," whether they are true or not.
1. Assume Their PMS Symptoms Are Universal or Deserved
While PMS is very common and seems to affect the majority of people who menstruate, it is not a universal condition. It is estimated that about 3/4* of menstruating people experience PMS at some point in their lives. 1/4 don't, and people who have effective treatment often stop experiencing symptoms.
While the majority seem to be affected, that is not a reason to forgo seeking treatment if you find PMS symptoms adding challenges to your life. There are options in both the conventional and naturopathic systems that work quite well at symptom reduction or cessation.
2. Dropping All Carbohydrates From Their Diet
Carbohydrates are useful in moving tryptophan across the blood-brain barrier. Tryptophan is used to make melatonin and serotonin, brain chemicals that help you sleep and be happy. Consuming carbohydrates has been shown to reduce the symptoms of PMS, in particular, whole grains, but increasing overall carbohydrate intake was also effective in studies that did not include whole grains.
The bottom line is that whole grains helped, but so did non-whole-grain carbohydrates. Over-fueling can also lead to worse PMS symptoms, so increasing carbohydrate intake should be done with care and may not be right for everyone.
3. Drinking Too Much Alcohol
Women with PMS tend to drink more. There is debate about whether having PMS causes women to drink more or whether drinking more causes PMS.
A meta-analysis is one of the best kinds of studies. It eliminates some bias and pools data from multiple studies to bring us closer to the truth. A meta-analysis published in 2017 found that women who consumed an average of one drink per day were 45% more likely to have PMS compared to non-drinkers. Women who consumed more than 8 drinks per week were 79% more likely to have PMS.
This is a pretty substantial increase, but keep in mind, greater than 8 drinks per week can be an average of people who had just 8 drinks per week and people who drank substantially more. What we can conclude from this study is that drinking more is associated with a greater risk of having PMS. Association does not equal causation, but a dose-response effect was found here, so it seems likely.
Another study found similar results. Women who consumed more than 10 drinks per week were more likely to suffer from moderate to severe PMS symptoms compared to non-drinkers.
One small study took women with severe PMS and women with no PMS and injected both groups with alcohol during the follicular phase and during the luteal phase. They measured a PMS-related hormone, allopregnanolone, and found that when alcohol was injected during the luteal phase (last half of the cycle) it caused allopregnanolone to fall in both groups. This fall was not seen in the follicular phase (first half of the cycle). Allopregnanolone is involved with the mood-related symptoms of PMS. This study showed that alcohol can change the levels of a PMS-related hormone in women with and without the condition.
In a perfect world, we would have randomized controlled trials comparing many different levels of alcohol consumption on PMS symptom severity, but we don't have that at this point. We have enough information to know that alcohol consumption is likely a contributor to PMS, and heavy drinking is more harmful than light drinking, but I don't have the evidence to back exactly how many drinks would be "safe" or not contribute to effects.
*I know about that one Canadian study that claims 99% of women experience PMS. Some studies use a broader definition of PMS or have a different methodology than other studies. Different studies find different prevalence rates, but 99% seems like an outlier. However, as more studies are done and more data collected, I expect these numbers will change a bit over the years.
© 2025. All rights reserved.
Disclaimer: All content on this website is for informational purposes only, does not constitute medical advice, and does not establish any kind of patient-doctor relationship by your use of this website. A patient-doctor relationship is only established after we have expressly entered into a written agreement with you that you have signed the consent forms, including our fee structure and other terms to represent you in a specific matter. Although we strive to provide information that is accurate, the information presented here in not a substitute for any kind of professional advice and you should not rely sole on this information or expect it to apply to your specific situation. Always consult a qualified professional for your particular needs.
